Table of Contents (click to expand)
An autoclave is a machine that is used to eradicate biohazardous waste from the surface of tools or instruments. It was invented by Charles Chamberland in 1884. Autoclaves sterilize or disinfect through physical means by using pressure, temperature and steam. They are often referred to as steam sterilization machines.
Sterilization is a quintessential process of any medical procedure, such as surgeries. Surgery renders its involved instruments contaminated with harmful microorganisms that can be life-threatening if reused on another patient without cleaning them first.
Other than surgery, sterilization is also mandatory for seemingly less important procedures, such as dental check-ups or to prevent the spreading of fungal infections in nail salons by regularly cleaning the tools used for manicures and pedicures.

A more palpable example is the boiling of water or cooking food in pressure cookers. Pressure cookers operate at sweltering temperatures and very high pressures to kill every last microorganism that colonizes and feasts on raw food.
Similarly, medical labs use a highly meticulous and effective machine that operates on a similar principle to kill biological waste – an autoclave.
Recommended Video for you:
What Is An Autoclave?
An autoclave is a machine that is used to eradicate biohazardous waste from the surface of tools or instruments. It was invented by Charles Chamberland in 1884. Autoclaves sterilize or disinfect through physical means by using pressure, temperature and steam. They are often referred to as steam sterilization machines.

Microbes on medical or scientific instruments cannot simply be cleaned with water or swept away with a brush or cloth. They require extra care because microorganisms and germs are highly resilient and impervious to these frivolous attempts of cleansing. They can only be eliminated by killing them, which is done by subjecting them to harsh environments.
An autoclave, with the help of a cloud of steam and elevated pressure, maintains a temperature that is too high for any bacteria, virus, fungi or parasite to survive in. However, other than these germs, spores are microscopic varmints that are indifferent to high temperatures. Fortunately, they can be eliminated if these extreme conditions are maintained for a prolonged period of time.
Autoclaves are basically used in any field where tools come in contact with biological matter. This would include tattooing, podiatry, funeral homes and prosthetics.
How Does It Work?
As mentioned, an autoclave is tantamount to a pressure cooker. The difference is that autoclaves are much more severe in their action.
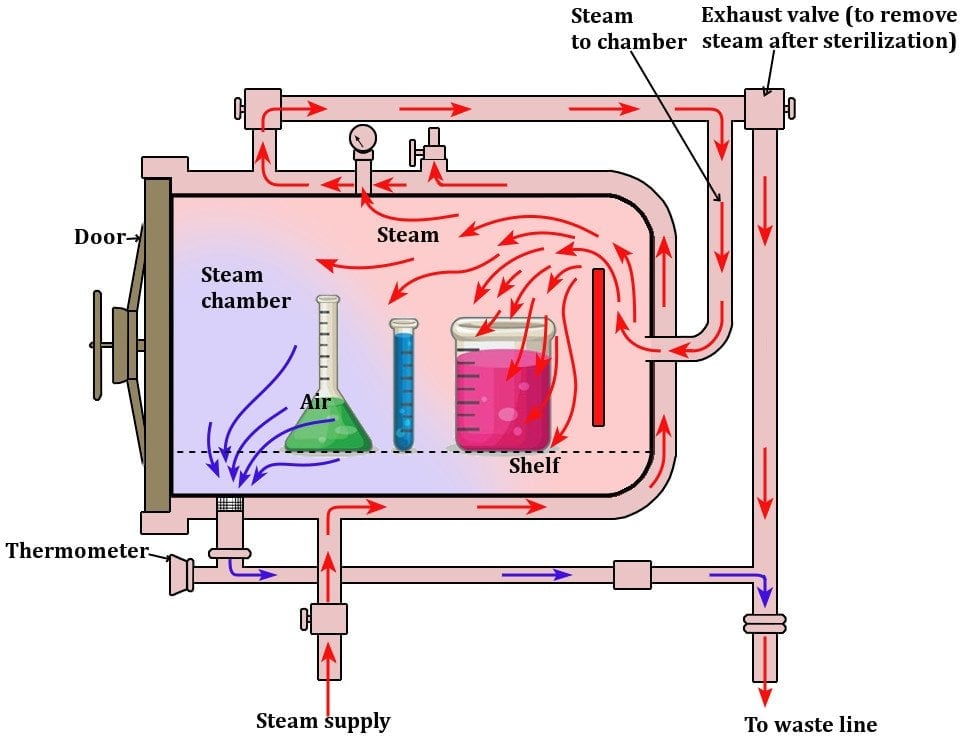
The instruments to be sterilized are stored in a chamber in the belly of the autoclave. As soon as the autoclave is switched on, a dense cloud of steam is fed into the chamber. At that point, the pressure and temperature begin to increase. Generally, most autoclaves aspire to maintain a temperature of around 120 °C (about 250 °F).
The apparatus also includes multiple valves and pipes to allow the steam to enter the chamber and steer the contaminated air towards the exit. Moreover, the application of the particular combination of 120 °C and 15 minutes is not obligatory. Different combinations are used depending on the materials inside.
For instance, autoclaves have been known to apply a combination of 134-138 °C for 3 minutes. Similarly, other suitable combinations can also be used.
These conditions are maintained for about 15 minutes, which is enough time to kill every microorganism and all the spores. The process destroys the internal parts of a microorganism and effectively ceases its existence. After the necessary time has elapsed, the steam is removed, and pressure is gradually decreased.
The process is based on displacing the contaminated air in the chamber with saturated steam and forcing this steam to persist so that the extended exposure can ensure effective sterility. It is to be carefully noted that the steam is neither superheated nor allowed to contain more than 5% moisture.
The procedure can be executed in two ways, formally known as autoclave “cycles”. The first one is Gravity or fast exhaust, in which the chamber endures high pressure and temperature for a particular period of time; at the end of this period, the valve is opened and the chamber swiftly returns to atmospheric pressure. This method is used to clean dry goods or glassware.
The second cycle is known as Liquid or slow exhaust. The cycle prevents a sterilized liquid from boiling. The steam is exhausted slowly at the end of the cycle, gradually cooling the superheated liquid. The cycle is primarily used for liquids, as the name suggests, but it can also be used for certain other materials.
One must ensure that safety measures are religiously followed, such as the use of gloves throughout the entire procedure and avoiding harmful burns by not touching the insides of the chamber while handling the articles inside.

The instruments are sterile and disinfected until they are utilized again. The autoclave now awaits them until they’re done being used. The process must provide a Sterility Assurance Level (SAL) of 10^-6 or better.
Even though the autoclave is one of the go-to techniques for sterilization, many materials are strictly recommended not to be autoclaved. These include acids, bases and organic solvents. Non-stainless steel, chlorine, seawater, sulphates, and bleach are other materials that are also highly incompatible and consequently dangerous to feed an autoclave.
The advent of sterilizing instruments is fundamentally important in poverty-stricken countries due to their lack of excess tools, which forces them to reuse perceptibly “clean” tools. This act could be fatal in some instances and must be avoided at any cost.
Some governments are speculating on the use of solar-powered autoclaves to mitigate their health risks, as well as assuage their financial plight.

Also, advancements in technology have led to the introduction of innovative waste converters, which can accomplish what an autoclave does without elevated pressure in order to sterilize rubber materials, such as gloves, gowns, dressings etc.
This is particularly useful for materials that are strictly required to be sterilized but cannot endure the high temperatures of an autoclave.